Affiliates with Red Mojo
Red Mojo is accepting new affiliates through the end of the quarter. The application takes 90 seconds.
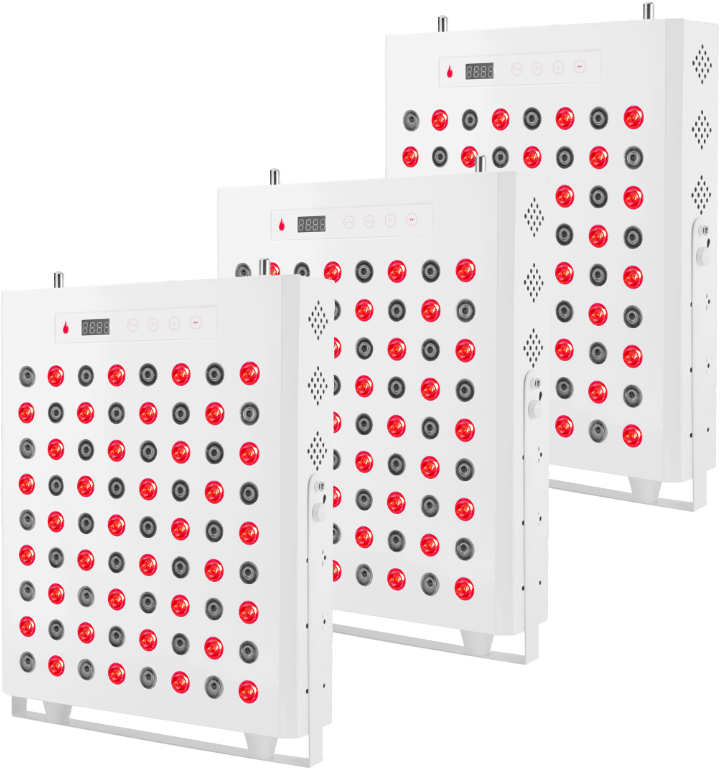
Red Mojo Benefits

Get 50% for a test product
As an affiliate, you can get a 50% discount on our product to test it. This discount can’t be cumulated or use on a product that you want to resell.

Up to 25% comission
Red Mojo is offering a top range of affiliates commissions, it allows our affiliates to earn a decent amount of money while promoting our product.

x4 What you can get on Amazon
Red Mojo earns you WAY more commission than Amazon links!

Get Custom Coupon Code
For special events or flash sales, Red Mojo is offering coupon code that benefits your customers.
Sell a Product backed by Science
1
More than
+3500
Research paper published
2
In which
+73%
Shown positive outcome
3
With
620-850nm
As the most studied wavelength
Radiation at 810 nm (5 J/cm(2)) given before or after TNF-alpha decreases the mRNA level of TNF-alpha and IL-1beta in RA synoviocytes. This treatment using 25 J/cm(2) also decreases the intracellular levels of TNF-alpha, IL-1beta, and IL-8 protein but did not affect the levels of seven other cytokines/chemokines. TNF-alpha-induced activation of NF-kappaB is not altered by 810 nm radiation using 25 J/cm(2).
We conclude that photobiomodulation therapy was able to promote the reduction of proinflammatory cytokines such as TNF-α and CINC-1, to reduce the gene and protein expression of the bradykinin receptor (B1 and B2), as well as increasing the stimulus-response threshold of pressure in an experimental model of acute osteoarthritis.
The effects of the 18 J/cm2 dose of PBM were promising in reducing pain and neutrophil activity in knee samples, together with reducing oxidative stress damage in blood serum and spinal cord samples. PBM improved the antioxidant capacity in blood serum and brainstem, and decreased the knee pro-inflammatory cytokine levels.
Eight studies were selected from 68 original articles targeted on laser irradiation and oxidative stress. Articles were critically assessed by two independent raters with a structured tool for rating the research quality. Although the small number of studies limits conclusions, the current literature indicates that photobiomodulation therapy can be an effective short-term approach to reduce oxidative stress markers (e.g., thiobarbituric acid-reactive) and to increase antioxidant substances (e.g., catalase, glutathione peroxidase, and superoxide dismutase).
Our outcomes show that PBMT applied before and after endurance-training exercise sessions lead to improvement of endurance three times faster than exercise only.
Three moderate- to high quality double-blinded, randomized placebo-controlled trials and two low- to moderate quality translational studies performed on rats were included in this CAT. All 5 studies supported the use of PBMT over cryotherapy as a treatment for post-exercise muscle recovery following exercise. PBMT was superior in reducing creatine kinase, inflammation markers, and blood lactate compared to cryotherapy following strenuous/high intensity aerobic or strength muscular exercise. PBMT was also shown to improve post-exercise muscle performance and function more than cryotherapy.
It was evidenced that 75% of doses that presented positive results for performance enhancement in large muscle groups were between 60 J and 300 J, and that 85% of doses that presented positive results for performance enhancement in small muscle groups were between 20 J and 60 J (Fig. 1).
Four azoospermic and 16 oligospermia male patients were treated with a 6mW He-Ne/2.5 mW pulsed GaAs diode laser with a dose of 1.3 J/cm2. Although no improvement was noted in the azoospermic subjects, the sperm count increased from 2 to 5 times in the oligospermia subjects. In addition. ejaculation of abnormal spermatozoa decreased in several subjects. Libido also increased in 15 of the 20 patients. From these findings, it was concluded that LLLT offers a possible treatment for the oligospermia patient. particularly for the subfertile.
The literature review showed that LLLT is beneficial in treating male infertility. The laser can significantly improve the survival, motility, and speed of movement of spermatozoa. Laser therapy of patients with prostatitis and vesiculitis can eliminate infiltrative-exudative changes, improve reproductive and copulatory functions. Local illumination of red (635 nm) and infrared (904 nm) spectra should be combined with intravenous laser blood illumination (ILBI) of red (635 nm) and ultraviolet (UV) (365 nm) spectra.
The use of 830 nm LLLT in the proximal priority technique at the parameters used in the present study, on its own or as an adjunct to other techniques, resulted in successful induction of pregnancy in just over 21% of severely infertile females, with a substantial number of these achieving live births.
Irradiated cells demonstrated a higher proliferation rate and increased migration ability associated with a moderate increase in ROS production without a significant increase in oxidative stress and oxidative stress-activated processes. Near-infrared light stimulated mitochondrial oxygen consumption and ATP synthesis in HECV cells. Short near-infrared irradiation did not affect the viability of HECV cells, rather led to a stimulation of wound healing rate, likely sustained by ROS-mediated stimulation of mitochondrial activity.
ATP was determined at 10 min after laser application. The quantity of ATP in laser-treated cells was 7513 +/- 970 units, which was significantly higher (p < 0.05) than the non-treated cells, which comprised 3808 +/- 539 ATP units.
A new generation of light-emitting diodes (LEDs) has appeared as the result of a spin-off from the US NASA Space Medicine Program, which is much more powerful than the previous generation with quasimonochromatic outputs. These LEDs can offer target specificity to achieve photobiomodulation enhanced action potentials of the skin cells, in particular mast cells, macrophages, endotheliocytes, and fibroblasts, plus increases in local blood and lymphatic flow, in a noninvasive, athermal manner.
Currently, there is a wide range of lasers and devices available for the regeneration and healing of the skin. Lasers and light sources for skin rejuvenation involve the removal of aged skin tissue via thermal heat from high-powered lasers, stimulating the surrounding tissues to recover through natural wound-healing processes. In contrast, photobiomodulation, which makes use of low energy lasers or light-emitting diodes, uses no heat and has shown positive effects on the reduction of wrinkles and improving skin laxity.
PBMs lasers mainly utilize red and near-red light spectra to activate biological processes used in a wide range of medical applications (Table 2). Low-power sources as LEDs, broadband lights, and lasers are the sources of the photochemical and photophysical phenomenon without thermal reactions. Photon energy is converted to stimulate biological reactions as collagen synthesis. Near-infrared irradiation assists fibroblasts in making collagen to increase the consistency of the skin.
Twenty-five relevant articles (13 in vitro and 12 animal studies) were included. Eleven in vitro studies showed positive results with regard to the acceleration of cell proliferation and differentiation. All animal studies showed improved bone healing in sites irradiated with a low-intensity laser.
This systematic review was performed based on PRISMA guideline. Among these studies, five articles reported in vitro results, twelve articles were in vivo, and three of them were clinical trials (…) PBM’s effects depend on many parameters which energy density is more important than the others. PBM can significantly enhance expression of osteocalcin, collagen, RUNX-2, vascular endothelial growth factor, bone morphogenic proteins, and COX-2.
Low-level laser rays cause brown adipose fat droplets to coalesce and fuse. Additionally, they stimulated the proliferation and congestion of capillaries in the extracellular matrix.
Ten of 11 trials demonstrated significant improvement of the androgenic alopecia in comparison to baseline or controls when treated with LLLT. In the remaining study, improvement in hair counts and hair diameter was recorded but did not reach statistical significance. Two trials did not include statistical analysis but showed marked improvement by hair count or by photographic evidence. Two trials showed efficacy for LLLT in combination with topical minoxidil.
At the present time, several different PBM devices are marketed to assist with hair regrowth in alopecia patients. This review covers the three main types of alopecia (androgenetic, areata, and chemotherapy-induced), and discusses the mechanism of action of PBM for each disease. The different devices used (mostly low powered red laser diodes), dosimetry, animal models, and clinical trials are summarized.
Low-level laser light therapy is a promising new treatment modality for AGA. The RCTs reviewed in this study highlights these benefits. It has proved to improve hair thickness and density with very few tolerable side effects. In addition, patients were satisfied with the results. There is a need for larger RCTs, especially comparing it to the standard treatment modalities like finasteride and minoxidil.
LLLT promoted statistically significant changes in NO release and MTT value only at the wavelength of 660 nm (p < 0.05). LLLT also promoted an increase in the NO release and cell viability when the energy densities 64 (p = 0.04) and 214 J/cm2 (p = 0.012), respectively, were used.
Many studies have shown that PBMT has positive photobiostimulatory effects on bone regeneration, accelerating its process regardless of parameters and the use of biomaterials. However, standardization of its use is still imperfect and should be better studied to allow correct application concerning the utilization protocols.
Low-level laser rays cause brown adipose fat droplets to coalesce and fuse. Additionally, they stimulated proliferation and congestion of capillaries in the extracellular matrix.
Non-irradiated control animals display inflammatory areas almost five times greater than the treated group (p < 0.001). This result on inflammatory infiltrate may have caused impacts on the significantly lower blood glucose level from irradiated animals (p = 0.04), twenty-four hours after the last irradiation session.